Summary
Cannabis has a long history of human consumption – it has been used as a natural remedy for a number of health conditions. In the UK, medical use of cannabis was legalised in November 2018. Despite this, only a small amount of British patients so far have benefited from the cannabis industry getting the green light. Patient access remains sluggish, and a limited amount of cannabis products are prescribed by the NHS. Project Twenty21 is a registry related to medical cannabis, and has so far enrolled 20,000 patients. It aims to promote patient access to medical cannabis and gather valuable evidence of medical cannabis’ efficacy.

Introduction
In November 2018, the UK legalised cannabis for medical use, following the cases of two children named Billy Caldwell and Alfie Dingley, who suffered from severe epilepsy and claimed to gain significant relief from cannabis. Despite the law change, access to medical cannabis in the UK remained minimal for most people. The challenges are related to the lack of scientific evidence on cannabis benefits, the high price of medical cannabis, and the lack of doctors ready to prescribe cannabis to their patients. Project Twenty21, monitored and created by Drug Science, is a way to expand access to medical cannabis to all people that may get relief from this medicine. In this post, we will see how patients and prescribers can join the project and what benefits they may get from it.

Cannabis as a medical treatment
The Cannabis sativa plant contains over 100 chemicals known as cannabinoids. Of these compounds, cannabidiol (CBD) and delta-9-tetrahydrocannabinol (THC) have undergone the most detailed scientific research, and their therapeutic potential is the most well-known. These compounds may interact with the body’s endocannabinoid receptors and adjust neurotransmitter function in the brain, potentially impacting physiological functions, from pain and inflammation to memory and sleep issues.
THC is psychoactive, resulting in temporary changes in a mood and behaviour, known as ‘high’ effect. For that reason, THC is a controlled substance under the UK Misuse of Drugs Act 1971. On the other hand, CBD is the second most common cannabinoid, and is non-psychoactive, and generally well-tolerated in humans. For that reason, there is a variety of different CBD products, ranging from CBD oils and tinctures to CBD sweet treats, that may benefit various symptoms of health issues.
The interest in medical cannabis and its potential for a number of health conditions has led to a rise in its possible use for medical purposes, through medical cannabis programs or recreational markets. Among the most common reasons to use medical cannabis are symptoms of chronic pain, neurological disorders, and mood-related issues, such as anxiety and depression. The most significant point about cannabis is its legal status that varies in different countries; however, many countries are well on their way to legalising cannabis for medical purposes.
Source: Visual Capitalist

Medical cannabis in the United Kingdom
In November 2018, the cannabis plant was legally rescheduled in the UK, going from a Schedule 1 to become a Schedule 2 drug of the Misuse of Drugs Act in the United Kingdom (UK). This move allowed specialist doctors on the General Medical Council Specialist Register in the UK to prescribe cannabis-based medicines to their patients. The policy of cannabis legalisation for medical purposes gained significant support from the British population, as many people may benefit from its use.

Source: The Lancet
For example, up to 400 thousand patients with rheumatoid arthritis in the UK could relieve their pain and discomfort from medical cannabis. As of 2020, three cannabis-based medications can be prescribed and considered legal for use in the UK:
- Epidiolex, a CBD-rich liquid used to treat rare forms of epilepsy in adults and children, such as Lennox Gastaut and Dravet syndromes, and multiple sclerosis.
- Sativex, a mix of CBD and THC used for treating spasms and muscle spasticity in multiple sclerosis.
- Nabilone, a synthetic form of THC in a capsule form, is used to treat nausea and vomiting, which can be caused by chemotherapy as a treatment for cancer.
All other cannabis-based medications are unlicensed and are also known as “specials.” These medications can be prescribed for an individual patient’s exceptional needs if no licensed ‘mainstream’ alternatives are available.
Currently, there are two ways to receive the cannabis-derived medications:
- Get prescriptions for licensed medical cannabis with NHS coverage
- Get private prescriptions without NHS coverage
Despite legalisation, access to medical cannabis and the number of cannabis-based medications in the UK has remained low. According to the 2019 Care Quality Commission report, only 18 cannabis prescriptions were given through the NHS in 2019, despite medical cannabis’s supposed availability as of 2018. In the case of private health care, there were just 259 private prescriptions in the same year.
The common factors that restrict access to medical cannabis in the UK include:
- Lack of valid scientific evidence on cannabis’ purported therapeutic effect
- The high price of medicinal cannabis products
- Insufficient training on medical cannabis for doctors
Doctors tend to prescribe medical cannabis when other, more familiar treatments are not helpful. Due to a lack of approved cannabis-based medications and limited indications, not many people in the UK are prescribed medical cannabis. Not to mention, medical cannabis is expensive. The cost of Epidiolex ranges from £5,000 to £10,000 per patient annually, while for Sativex it’s more around £2,000 per patient annually. The NHS’s indicative price for Nabilone reaches £196 for 20 packs. Private prescriptions is an easier route, but these are also more costly and suit patients who can afford up to £250 for private appointments and from £600 to £800 for prescriptions each month.

A prohibitionist approach to medical cannabis in the UK can make patients turn to the illicit market. It is hoped that data from Project Twenty21 will help improve patient access to medical cannabis in the future. Additional research may help convince doctors of medical cannabis’ effectiveness. Randomised controlled trials (RCTs) are viewed as the gold standard, as they deliver the highest level of acceptable scientific evidence; however, the therapeutic potential of cannabis and its availability in many countries presents an opportunity to collect real-world data (RWD).
RWD aims to evaluate the effects of health interventions that are not collected in the standard highly-controlled trials and reflect how these interventions might be used in routine clinical practice.
What is Project Twenty21?
Project Twenty21 (T21) is the largest medical cannabis patient registry in Europe that has gone live in August 2020. The project will enrol 20,000 patients taking medical cannabis for specific health conditions and monitor the health outcomes till 2021. The registry will help create Europe’s largest body of evidence relating to these medicines’ safety and promote the integration of cannabis into mainstream UK healthcare.
Drug Science, the UK’s leading independent scientific body on drugs, has initiated Project Twenty21 intending to provide evidence that the possible benefits of treatment with medicinal cannabis likely outweigh the potential risks, and that medical cannabis should be available for NHS funding. The thing is that private medical prescriptions are high-priced, and can create a barrier for patients seeking treatment. The findings of the project may help promote future medical cannabis policy and improve the number of prescriptions. The project will be available for patients with a limited number of health conditions, which means that not all patients in need will be able to take part.

Who can participate in Project Twenty21?
To participate in the project, patients must provide the chosen clinic, excluding Drug Science, with both:
- Confirmation that the patient has one or more of the following conditions they would like to supplement with medical cannabis use:
- Chronic pain
- Multiple sclerosis (MS)
- Anxiety disorder
- Post-Traumatic Stress Disorder (PTSD)
- Tourette’s Syndrome
- The information, proving that a patient has tried at least two different medications that have been unsuccessful at managing the health condition. This information must be provided in a medical summary, or a referral letter from the GP practice.
What conditions are included in Project Twenty21?
There is a limited number of conditions that may be covered by Project Twenty21. The creators of the project aim to evaluate the possible benefits of cannabis for six specific conditions.
Chronic pain
Based on the most credible studies, up to 43 per cent of the UK population suffers from chronic pain, which equals 28 million people. A 2019 GlobalData cannabis consumer research paper has shown that half of all cannabis consumers use it to potentially reduce pain. Chronic pain is incurable in common knowledge, but may be alleviated. Although cannabis can not relieve severe pain, such as post-surgical pain, it may help with chronic issues. Medicinal cannabis products might be safer than opiates, as they are more difficult to overdose and will not get you addicted. Studies show that cannabis might cause pain-relieving effects. Additionally, opiates may cause a sedative effect, while medical cannabis is generally well-tolerated.
Medical cannabis has demonstrated some efficacy when it comes to reducing neuropathic pain. Some studies show that medical marijuana in low-doses may help alleviate neuropathic pain if used with other analgesic medications.
Anxiety
Anxiety is an emotion or condition related to feeling restless, nervous, or tense. Anxious people consider most situations as threatening. The feeling of worry and uneasiness may cause muscular tension, fidgetiness, fatigue, and concentration loss. In 2013, 8.2 million people suffered from anxiety disorders in the UK. Where some patients prefer natural supplements, cannabis has become a potential option. Cannabidiol (CBD) may interact with endocannabinoid receptors in the central and peripheral nervous systems, causing an anxiolytic effect. Cannabidiol may also interact with serotonin receptors, which play a crucial role in your mental health. Studies have found the potential ability of CBD to improve the symptoms of anxiety and promote better sleep. Considering the complexity of anxiety disorders and the variety of cannabis-based medications, further research is needed.

Post-Traumatic Stress Disorder (PTSD)
A mental health condition provoked by surviving a traumatic event, such as warfare or natural disasters, develops in some people who experience extreme stressors, such as military and veteran populations. Such a condition is commonly treated with a combination of medication and therapy, including cognitive behavioural therapy. Studies have found that oral administration of CBD may cause a beneficial effect for patients with PTSD, including possible relief in patients with frequent nightmares.
A review of cannabis use for mental health also suggests other benefits for individuals diagnosed with PTSD, including reduced irritability, restlessness, sleep difficulties, and improved emotional regulation and reduced anxiety. Recent studies have suggested the ability of CBD to reduce the effect of aversive memories and promote improvements in the symptoms of PTSD. CBD can be taken as a supplement to cognitive behavioural therapy.
Multiple sclerosis
Multiple sclerosis is a disabling disease of the brain and central nervous system that results in an autoimmune response damaging nerve cells’ covers. This can potentially lead to progressive neurodegeneration and disability, and worsen the quality of life for a long time. According to a 2010 study, up to 127,000 people in the UK suffered from multiple sclerosis. Sativex, an oral spray containing a mix of THC and CBD, is licensed for treating the common multiple sclerosis symptoms, such as muscle stiffness and spasms. Sativex was shown to be effective in treating muscle spasticity and in improving the quality of life. Additionally, a low incidence of Sativex-related side effects supports its good safety profile and tolerability.
Tourette’s syndrome
Tourette’s syndrome is an inherited, neurological condition that causes multiple involuntary motor and vocal tics. This condition often begins in childhood and affects up to 1% of school-aged children and 0.3%-0.5% of adults in the UK. There’s no cure for Tourette’s syndrome. Tourette’s syndrome treatment focuses mainly on reducing or controlling the tics and other symptoms through behavioural, rather than medicinal treatment, due to potential side effects of medications used. Studies show that cannabinoids may be effective in the suppression of tics and help with associated behavioural problems. Cannabis use may positively affect aggression, improve symptoms of anxiety and sleep, and lessen the difficulty of falling asleep. Cannabis may positively impact patients with Tourette’s syndrome; however, further studies are needed.
Substance use disorder (SUD)
Also known as drug addiction, SUD impacts a person’s brain and behaviour and results in an inability to control the intake of legal or illegal drugs or medications. If you’re addicted, you may continue taking the drug despite the potential harm to your health. In the UK, 3 percent of the population have a substance use disorder. Treatment of drug addiction may include therapies, medications, detoxification, and support groups. Preliminary scientific evidence suggests that medical cannabis may be useful for managing substance use disorder. For example, CBD may inhibit some of these brain reward mechanisms that increase the opioid reinforcing properties. Studies show that cannabis may become a safer alternative for alcohol, illegal drugs and pharmaceuticals due to less harmful side effects, low-risk for addiction and effectiveness at alleviating symptoms, such as chronic pain. Additionally, many people with cannabis use disorder become addicted to strong cannabis, such as skunk, which is low in CBD. Using THC-low plant extract might also help these people to reduce their high THC use.
What are the side effects of medical cannabis?
The most common side effects following medical cannabis intake include:
- Red eyes
- Low blood pressure
- Dizziness
- Increased heartbeat
- Depression
- Hallucinations
- Altered judgment and coordination
Inhaled cannabis products may also compromise lung health. Studies show low toxicity of medical cannabis and low risk of addiction if taken in therapeutic doses. Medical cannabis with higher THC level also carries a low risk of addiction if taken regularly for chronic conditions, and the risk is lower than with opioid pain medications and other drugs taken for anxiety and sleep. Moreover, T21 participants undergo an assessment every three months, which helps to detect any adverse effects and control any signs of addiction.

What medications can be used for the project?
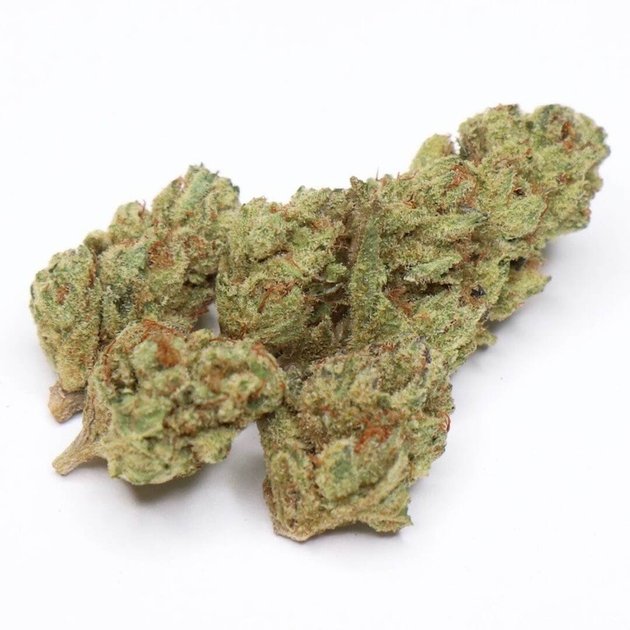
Project Twenty21 works with a network of private clinics and licensed producers, including Senzer Pharmaceuticals, Lyphe Group, Bod Australia ltd, Khiron Life Sciences, Cellen Therapeutics, and Jamaican Medical Cannabis Corporation to provide cannabis-based medicinal products of the highest quality. The Project Twenty21 includes Indica & Sativa flower products with different CBD : THC ratios, various oils, and alternative options, such as a synthetic medication. The T21 formulary includes flower, oil, and vape products from T21 license producers.
Only the products of these formularies will be subsidised at £150 per product per month, and the amount is limited according to dosage guidance from the Medical Cannabis Clinicians Society. The patient must pay the remaining amount. In general, medication, dosage, and costs should be discussed during a consultation. Smaller dosages at lower prices are available.
However, some cannabis-based medications (CBMPs) prescribed by the clinician will not be subsidised via Project Twenty21. As Twenty21 products do not meet a patient’s needs, doctors are allowed to prescribe whatever product is available and suits the patient’s condition best. Patients can accept these medications and pay the full price, or refuse the prescriptions if the cost is too high. The doctor who prescribes medicinal cannabis will send the Twenty21 prescription to the pharmacist. Then, patients pay for the medication, dispensing, and delivery. To receive subsidised medications, patients must agree that Drug Science will collect their medical data. This information will be used to evaluate the potential benefits and side effects of CBMPs and kept confidential. After the payment, medication will be sent to the patients’ address.
Patients’ information
Have an interest in the project? Here is what you should do:
Before the consultation
First, you should contact the clinic and inform them that you would like to participate in Project Twenty21 and receive subsidised products. Medicinal cannabis consultations are not aimed to diagnose a condition; however, some clinics offer an additional appointment and a pre-assessment for a review of patient healthcare records at a charge. It is important to note that prescription products that are not included in Project Twenty21 will not be subsidised and will incur prescription, dispensing, and delivery costs.
Attending the consultation
There are two ways to get the consultation – remotely, via telemedicine, or face-to-face. It would be best if you also inform your doctor about your wish to participate in Project Twenty21. The doctor will conduct an initial assessment and fill in a questionnaire, including:
- Diagnoses
- The information on previous and current medications and therapies taken for any health condition(s)
- How symptoms impact the patient’s quality of life, such as their mobility or sleep
- Any data on previous cannabis-based products and cannabis use, including the most effective medication, the type of the product used, and side effects
After checking the patients’ medical history and condition needs, the doctor will conclude whether to prescribe medicinal cannabis products or not. Therefore, attending a consultation is not a guarantee for a medical cannabis prescription.

After consultation
Clinics will decide on the regularity and cost of follow-up consultation, including the data collection every three months. Follow-up consultations are a necessary condition to receive the medication.
How to choose a clinic
Project Twenty21 has cooperated with a network of private clinics, such as Medical Cannabis Clinics, to collect health outcome data. A clinic refers to doctors and healthcare practitioners, with diverse expertise and specialities. Before contacting clinics, patients should determine whether that specific clinic can handle their health condition. Patients should also inform clinics that they would like to join Project Twenty21 before the consultation. Patients fund the cost of their consultation, which varies between clinics. The clinics and initial consultation fees are listed on the Drug Science website to help patients choose the clinic they would like to register with. Consultations are not intended to diagnose health conditions, but to define whether medical cannabis would be appropriate for a diagnosed condition.
How to track your progress
Alta Flora, a digital therapeutics company and a founding industry partner of Twenty21, has created Eva’s app for patients taking cannabinoid medications. Eva allows patients to record their symptoms, any possible interactions with other drugs, and collect valuable data on the safety and effectiveness of medical cannabis, such as medication routes of administration, including dose and formulation, through their phones. With the use of validated scales and questionnaires, users may explore trends and assess their quality of life. Eva also provides tools for researchers to conduct studies with clinics and capture data on their own patients. An app is an opportunity to collect data, such as real-time reporting dashboards, to help clinicians, prescribers, and regulators to understand the effect of cannabis on patients’ symptoms and their quality of life in a more detailed way. The platform producers also hope that the platform could also be used to monitor the potential effectiveness of CBD products on anxiety, sleep, and pain. The service is GDPR-compliant, and will involve patient safety monitoring features. The app can be used on both iOS and Android.
Prescriber’s information
Who can prescribe medical cannabis?
Any doctor registered on the General Medical Council (GMC) is allowed to prescribe medical cannabis. A general practitioner (GP) can prescribe according to shared care arrangements and a specialist’s direction. However, the majority of NHS Clinic Commissioning Groups (CCGs) would rather not issue prescriptions from private clinics.
How to prescribe medical cannabis through Project Twenty21?
If you are a doctor with GMC registration and would like to prescribe medical cannabis via Project Twenty21, you should follow these steps:
- Join the project
There are three main options when you join the project:
- Choose any of the project’s clinics through Clinic Directory
- Prescribe as an independent clinician
- Work within your existing organisation
Clinics who would like to join T21 do not need to specialise in medical cannabis but rather have expertise in prescribing for a more specific condition, such as chronic pain. Additionally, independent clinicians are encouraged to join the project, though they aren’t listed on the project’s website. The clinics charge their own pricing for the initial assessment and follow-up consultations, and the patient covers these costs.
- Receive training
Prior to training, a clinician must sign a Memorandum of Understanding to confirm their adherence to T21 processes. Then T21 members set up a video call to demonstrate the project protocol. The clinician then receives a full Clinicians Onboarding Pack, including copies of the project protocol and formulary. There is also an option to connect with the Medical Clinicians Cannabis Society (MCCS) for additional educational materials. To collect the data on patients, the project organisers use an online system called Sail. A clinician will also get a live Zoom-webinar training to know how to use the system and receive a Sail login.
- Register a patient and conduct an initial assessment
Within the Clinician’s Onboarding Pack, a clinician also receives a Patient Informed Consent Form. Some extra documents need to be completed and confirmed before adding a patient on Sail:
- Confirmations of primary indication and eligibility to be prescribed medical cannabis (at the clinician’s discretion)
- Provision of informed consent
The above documents can be added by admin staff if they have received training on Sail. The patient should also complete a questionnaire(s) based on their primary indication before the initial assessment. Checking the patient’s data before the initial assessment helps to speed up a patient appointment time and decide on prescribing more quickly.
The project’s members ask to provide the patient with up-to-date product information and how-to guides on the product being prescribed, which should be available in the Sail system.
- Track the patient’s progress
To monitor the patient’s condition and the cannabis product effect, a clinician will need to conduct an assessment every three months over 24 months or as long as the patient takes part in a project. All patient data is collected through the Sail system.
Where should you look for additional support?
Joining the Project Twenty21 may sound challenging, though there are many options to get advice and support:
- Contact Drug Science via [email protected] to consult a Drug Science T21 team member to learn more about joining Project Twenty21
- Get educational resources and updates through the Medical Cannabis Clinicians Society to confidently prescribe and share clinicians’ knowledge
- Learn more about cannabis-based medical treatments and their potential for the patient’s needs through Primary Care Cannabis Network, a community platform and educational tool for general practitioners
CBD products for overall well being

Medical cannabis is designed to have the potential to ease symptoms of severe health conditions, such as symptoms of epilepsy and muscle spasticity. To get medicinal cannabis products, you need to have a provable need for cannabis use, get a prescription, and be ready to pay a lot for a medication. However, there are a number of less severe (though still discomforting) conditions, such as anxiety and stress, sleep loss, skin issues, and pain. CBD products may become an excellent way to support wellbeing and possibly ease daily tensions.
With so many low-quality and overpriced products on the market, getting high-quality, most reliable CBD products is challenging. In such a case, Alphagreen, one of Europe’s leading marketplaces for CBD brands and alternative healthcare products, comes to the rescue. Here, you can find CBD treats for the most demanding taste, ranging from traditional CBD oils and tinctures to all-natural sweet chocolates and soothing balms. Buying from Alphagreen means you get much more than a CBD oil or fruity CBD gummies. Here is why you can trust Alphagreen selection:
- CBD products are selected from only the world’s trusted CBD brands
- Certificates with lab results, confirming the products are THC-free and contain the stated level of cannabinoids
- Product reviews with an independent opinion
- Customer support, so you can make the best choice
- Convenient shipping and return conditions
- Blog posts based on the latest research for a better understanding of CBD’s potentially beneficial effects
Alphagreen takes your health and wellbeing seriously and carefully selects the best products for your needs. Your health is in good hands, and your choice is supported at each step, from deciding your dosage to choosing your very first CBD product.
Final Thoughts

Project Twenty21 is a silver lining in the cannabis world. Europe’s first medical cannabis goal is to create sufficient evidence supporting the potential of medical cannabis when it comes to managing specific conditions and demonstrating to policymakers that medical cannabis should become more affordable and available. The project results may also support prescribers in the UK to feel more confident in prescribing medical cannabis to their patients. Drug Science suggests that the findings of Project Twenty21 will provide a convincing case for NHS funding, showing the potential benefits of treatment with medicinal cannabis products outweigh the possible risks. Additionally, T21 may show that medical cannabis (which is now limited to a few areas of care) may possibly be used for a much more extensive range of health conditions.
The project will enrol only 20,000 patients with specific health conditions by 2021, which means that eligibility criteria may exclude some patients in need. The Drug Science team created a detailed plan for patients and prescribers alike to get all the necessary information and updates on the project. Therefore, if you fit the patient’s eligibility criteria, or would like to prescribe medical cannabis to the patients, you should check out the project.

Verified by a Healthcare Professional
Anastasiia Myronenko
Anastasiia Myronenko is a Medical Physicist actively practicing in one of the leading cancer centers in Kyiv, Ukraine. She received her master’s degree in Medical Physics at Karazin Kharkiv National University and completed Biological Physics internship at GSI Helmholtz Centre for Heavy Ion Research, Germany. Anastasiia Myronenko specializes in radiation therapy and is a fellow of Ukrainian Association of Medical Physicists.
Project Twenty21 is essentially the biggest medical cannabis patient registry in Europe. This project has been launched since August 2020, and will enrol 20,000 patients to consume medical cannabis for certain medical conditions so that they can be monitored for their health outcomes until the end of 2021. In essence, this project aims to help establish Europe’s largest source of evidence showcasing the safety of medical cannabis and thereby promote its integration into the UK healthcare system.
CBD is an abbreviation of cannabidiol, which is one of the 113 compounds that can be extracted from a species of plant known as Cannabis sativa. It is actually the second most common phytocannabinoid that can be found, alongside another chemical compound known as tetrahydrocannabinol (THC).
Volunteers who are looking to participate in Project Twenty21 need to have at least one of these medical conditions – chronic pain, multiple sclerosis, anxiety disorder, post-traumatic stress disorder, Tourette’s syndrome, and/or substance use disorder. In addition to that, the patient needs to have tried a minimum of two completely different medications that have been largely unsuccessful at treating their health condition. Crucially, this piece of information has to be confirmed by a certified general practitioner in order for the patient to fulfill the second criterion.
In short, CBD does not contain the psychoactive component that makes you “high”. Instead, the actual chemical compound that is responsible for that is another type of phytocannabinoid that can be extracted from the cannabis Sativa plant along with CBD called tetrahydrocannabinol (THC).
Some of the typical side effects of consuming CBD (usually in large amounts or incorrect dosages) include experiencing symptoms of lowered blood pressure, red eyes, an increased heart rate, dizziness, depression, hallucinations, an altered judgement, and/or lack of balance and coordination.