Summary
A comprehensive guide for those considering treatment with medical cannabis in the UK. In this article, the basics of medical marijuana are outlined, including it’s legal status, it’s deviation from recreational cannabis, it’s clinical uses, and it’s potential side-effects. We explore what public and private options are currently out there for individuals seeking to use cannabis to alleviate symptoms from specific conditions. To conclude, we look to the future of medical cannabis in the UK and predict how it’s administration in medical settings may expand in forthcoming years.
Introduction
When you think of the words ‘medical cannabis’, your mind probably jumps to Canada, or one of the 35 American states that have legalised the use of cannabis for remedial purposes. You wouldn’t be on your own. According to an ongoing poll carried out by Canex, up to half of adults in the UK are unaware medical cannabis is also legal on our home soil. But following the high profile cases of Billy Caldwell and Alfie Dingley, two children who saw their epileptic symptoms dramatically improve after the use of cannabis-based medications, the medical application of the drug was legalised in 2018. So, what does this mean for the rest of us?
With cannabis only being rescheduled from a schedule 1 to a schedule 2 drug in recent years, much is still unknown about its accessibility, the forms it comes in, it’s potential benefits, and it’s possible side-effects. Therefore, in this article, we attempt to dispel the myths around medicinal cannabis in the UK, to give you a clearer picture into what options may be open to you. In doing so, we’ll be taking a look at the incrececies of it’s legal status, exploring up-to-date research into it’s possible values, giving you a comprehensive rundown of what forms medicinal cannabis can come in within the UK, and assessing potential barriers to entry. But before we consider these issues, let’s establish the definition of medical cannabis first.
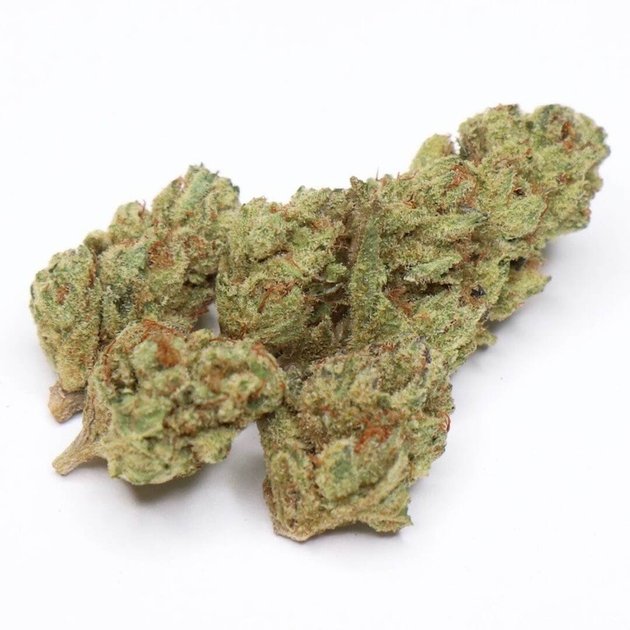
What is medical cannabis?
Medical cannabis or medical marijuana (MMJ), is a plant-based medicine made from cannabis Sativa or cannabis Indica. The medicinal herb is prescribed to patients who are looking to alleviate symptoms from a range of different conditions. Compared to other government-approved medications which typically contain just one or two compounds, a typical cannabis plant includes over 400 different chemical compounds, including over 120 cannabinoids such as cannabidiol (CBD) and tetrahydrocannabinol (THC). Therefore, the amount of active chemicals in cannabis is one of the reasons why it’s treatment is quite difficult to classify and study.
According to a recent survey, 43% of people in the UK with a disability or chronic illness haven’t used medical cannabis as they considered it illegal. Therefore, it’s high time to dispel doubts and to define what cannabis products are legal and allowed in the UK.

Is medical cannabis legal in the UK?
Since November 2018, the use of cannabis for medicinal purposes was finally approved for people living inside the UK. The legislation approved cannabis-based medicinal products as Schedule 2 controlled drugs according to the Misuse of Drugs Regulations 2001, which means they are currently available on prescription to patients who are deemed eligible.
The government has determined cannabis-based products for medicinal use as: “a preparation or product, other than one under paragraph 5 of part 1 of Schedule 4, which:
- Is or contains cannabis resin, cannabis, cannabinol or a cannabinol derivative (not being dronabinol or its stereoisomers)
- Is produced for medical use in humans
- is a medicinal product, a substance, preparation for use as an ingredient of, or in the production of an ingredient of, a medicinal product.”
Differences between medical and recreational cannabis
Even though both recreational and medical cannabis may of high quality, there are specific differences between them that should be considered:
Quality control and testing
Cannabis strains used for medical purposes undergo a more thorough process before becoming available for consumption and are usually grown in more controlled environments. The producers are obliged to follow Good Manufacturing Practices (GMP) and comply with other strict quality standards to sell it as medical cannabis. These practices include testing to ensure cannabis products don’t contain harmful components, such as pesticides and mould, but do contain the stated levels of CBD (cannabidiol) and THC (tetrahydrocannabinol). Moreover, it also ensures each batch is of equal quality. While recreational cannabis also undergoes stringent tests for heavy metals, microbial contaminants and cannabinoids content, the standards for recreational cannabis are lower than for the medical variety.
Purchase conditions
If you’d like to buy cannabis for medical use, you need to have a qualifying condition, get a prescription from your physician and make a purchase from a regulated dispensary or pharmacy. These rules also apply to the US, Canada and some European countries, such as Germany, Italy, Denmark and the Netherlands. Even though medical use of cannabis was legalised in the UK in 2018, it is still challenging to receive cannabis-based medications due to doctors’ reluctance to issue prescriptions and the low chances of receiving medications through the NHS. As for recreational cannabis, in Canada and 15 American states, its use is completely legal and it can be bought without medical recommendation.
In all countries, an individual should be over 18 to purchase cannabis and cannabis-based medications. As for the US laws, you need to be over 18 to buy medical cannabis from a dispensary and over 21 to buy recreational cannabis or marijuana from a dispensary.
Medical uses for cannabis
Chronic pain

According to GlobalData cannabis consumer research, in 2019, up to half of all cannabis consumers used it for pain treatment. Although cannabis isn’t strong enough to relieve severe conditions, such as post-surgical pain, it’s been shown to be useful for less severe cases of chronic pain.
As this study indicates, medical cannabis is being increasingly considered as a potential opioid substitute, particularly because the substance is understood to elicit analgesic effects while being much less addictive and sparing the risk of an overdose. Study participants reported improved pain and fewer side effects when treated with medical cannabis. It seems to relieve the pain caused by multiple sclerosis and nerve pain. Moreover, opiates may cause an excessive sedative effect. Patients report that medical cannabis allows them to carry on previous activities without feeling disengaged. There is also evidence that low-dose medical marijuana may alleviate neuropathic pain if used alongside traditional analgesics.
Neurological conditions
Neurological disorders include diseases of the peripheral and central nervous system, including headaches, epilepsy, neuropathic pain, Tourette’s syndrome, multiple sclerosis, Alzheimer’s and Parkinson’s disease. Cannabis for neurological disorders can be useful when treating pain, spasms and seizures, as well as anxiety symptoms such as depression, muscle weakness and decreased alertness.
Using medical cannabis for multiple sclerosis has shown some promising results. Numerous large trials using the combination of tetrahydrocannabinol (THC) and cannabidiol (CBD) as a drug Nabiximols/Sativex have shown improvements mostly in spasticity and pain, without changes in disability measures. Scientific research suggests cannabis-based medicines may reduce seizure frequency in epilepsy, and some clinical trials show benefit in specific pediatric epilepsy syndromes. There are also positive experiences with THC-treatment in children and adolescents with severe neurological disorders. Cannabis may be helpful in Parkinson’s disease, such as positive impacts on memory, mood, fatigue, and obesity. At the same time, side effects and paradoxical effects of medical cannabis depending on the amount of THC-like cannabinoids may exacerbate the treatment. Therefore, further research on cannabis effectiveness with neurological disorders is necessary.
Post-traumatic stress disorder (PTSD)

PTSD is an exhausting condition that is understood to affect around three in every 100 people in the UK. PTSD develops in response to a stressful, frightening or traumatic event, and symptoms include flashbacks, nightmares, hyper-reactivity, insomnia, and intrusive memories. Cannabis products have shown to reduce some PTSD symptoms such as nightmares and insomnia, and an array of studies conducted on animals also indicate that cannabis may be useful in the treatment of disorders such as PTSD.
Despite research into the therapeutic potential of medical cannabis for psychological disorders on humans being legally restricted, the limited research conducted on humans has suggested that cannabis might relieve particular PTSD symptoms. For example, a population-based cross-sectional study in Canada has shown that cannabis use may potentially reduce the association between PTSD and severe depressive and suicidal conditions. However since no conclusive information regarding the benefits of medical cannabis use in patients with PTSD is available and considering the lack of human studies with a sufficient number of participants, further studies are required before anything definitive can be concluded.
Nausea and vomiting
Medical cannabis has shown to be effective in chemotherapy-induced nausea and vomiting (CINV), a common side-effect of many cancer treatments. Studies have found cannabinoids may bring more benefits than some traditional antiemetics. Nabilone and dronabinol, orally-administered synthetic cannabinoids have been approved for the treatment of CINV. They act by blocking the binding of dopamine and serotonin, associated with CINV, at receptor sites. Cannabis-based medications can be prescribed to patients who don’t respond to common pharmaceuticals. As for natural cannabis, human trials have shown that it might be effective if synthetic cannabinoids failed. In addition to potentially alleviating nausea associated with CINV, natural cannabis is also useful for treating other types of nausea. And when medical cannabis is used to remedy general nausea, the therapeutic results depend on the THC concentration and THC and CBD ratios.
What are the side effects of medical cannabis?
The most commonly reported side effects include:
- Red eyes
- Low blood pressure
- Lightheadedness
- Depression
- Increased heartbeat
- Hallucinations
- Affected judgment and coordination
If used during the teenage years when the brain is developing, cannabis may affect IQ and mental function. Inhaled marijuana may increase the risk of bronchitis and lead to other lung problems.
Is medical marijuana addictive?
Most research has shown a low risk of cannabis addiction and low toxicity of medical marijuana if taken according to medical recommendations in small therapeutic doses. However, the US National Institute on Drug Abuse claims marijuana is considered a “gateway drug” to other drugs and may cause addiction. This statement is related to a higher THC level. Medical cannabis with higher amounts of THC carries a small risk of addiction if taken daily for chronic conditions. Still, this risk is lower than with opioid pain medications and benzodiazepines used for anxiety and sleep. Medical cannabis specialists monitor patients carefully to control any signs of addiction, minimise the risk and choose lower-risk products appropriate for patient’s symptoms. There is also concern about psychological dependence on cannabis in heavy users. Surprisingly, some research has shown CBD oil ability to treat marijuana addiction.
Who has the authority to prescribe medical cannabis?

According to the law, GPs are not allowed to issue prescriptions for cannabis-derived medicines. NHS guidance states that medical cannabis should be prescribed by a specialist consultant and in cases backed by clear published evidence of cannabis benefit and if other treatment options haven’t been helpful.
On November 11, 2019, The National Institute of Health and Care Excellence (NICE) published a guideline on Cannabis-based medicinal products and advice to clinicians. According to the guideline, medical cannabis should be prescribed by a specialist medical practitioner included in the register of specialist medical practitioners. Cannabis-based medications available for prescription and legal for use in the UK include Epidiolex, Sativex, and Nabilone. The doctors may also prescribe herbal medicinal cannabis products produced by Bedrocan BV, the Dutch government’s official manufacturer of medicinal cannabis. Bedrocan products, including Bedrocan, Bedrobinol, Bediol, and Bedica, are available on a private prescription. Cannabis products, such as dried flowers and whole-plant extracts are not available on the NHS, regardless of the severity of a health condition. Dronabinol, a synthetic cannabinoid, is not available as a licensed medicine in the UK.
It is also important to note that the recreational use of cannabis still remains illegal. Cannabis oil with more than 0.05 % of THC, the psychoactive element, is banned in the UK.
What medical cannabis is available in the UK?
NICE, an arm of the NHS, provided evidence-based advice and guidance on medical cannabis for health and social care practitioners. As of 2020, three cannabis-based medications are available for prescription and legal for use in the UK:
Epidiolex

Epidiolex is a drug created by GW Pharmaceuticals. The substance contains a highly purified liquid form of CBD used to treat rare forms of epilepsy in adults and children and multiple sclerosis, and is completely THC free. Following NHS approval, doctors can prescribe Epidiolex for children with Lennox Gastaut and Dravet syndromes, severe epilepsy that can cause numerous seizures a day. Out of the 3,000 people in England who currently suffer from Dravet syndrome and the 5,000 people who are living with Lennox Gastaut syndrome, approximately 2,000 people are expected to qualify for Epidiolex. NICE’s guidance followed the approvals of the European Commission in 2019, suggesting that Epidiolex should be used alongside the anti-epileptic generic drug clobazam (brand names Onfi and Sympazan) in the patients aged two and older.
The NICE guidelines were based on clinical trials and extension studies, evaluating its anti-epileptic efficacy, and safety for patients with Dravet Syndrome and Lennox-Gastaut Syndrome. Positive data gleaned from the studies suggested that Epidiolex treatment helped to cut seizure frequency in half while improving the general health of 80% of the participants. However, despite these victories, common side effects of Epidiolex during these trials included fever, sleepiness, appetite loss, vomiting, and diarrhoea.
Sativex
Also known as Nabiximols, Sativex is a mouth spray that contains a mix of CBD and THC. The drug has been approved for treating spasms and muscle stiffness, known as spasticity, in multiple sclerosis (MS). However, medical specialists are not allowed to prescribe Sativex to treat pain, which is often a debilitating symptom of MS. According to the Misuse of Drugs Act 1971, Sativex is a Class B controlled drug placed in less-restrictive Schedule 4 under the Misuse of Drug Regulations 2001. That means it can be prescribed legally in the UK without restrictions on supply, storage and destruction. However, Sativex can only be prescribed by a specialist doctor experienced in treating multiple sclerosis spasticity, such as consultant rehabilitation specialists, consultant neurologists and consultant pain specialists.
So far, the use of Sativex is limited to people who respond positively to the first four weeks of treatment. In case there is no apparent improvement in spasticity symptoms, the treatment with the drug is stopped. Common side effects of Sativex include drowsiness, dizziness, fatigue, diarrhoea, constipation, memory or concentration loss, dry mouth, and altered sense of taste. However, side effects are more likely during the first days of the treatment.
Nabilone
Typically administered in the form of a capsule, Nabilone is a drug used to treat nausea and vomiting caused by cancer chemotherapy. A doctor can prescribe Nabilone for symptoms relief, but only if other treatments have not helped with the condition or are not suitable. It is a synthetic form of delta-9-tetrahydrocannabinol (Δ⁹-THC) and acts in a similar way to THC. In Canada, the US, the UK and Mexico, Nabilone is marketed as Cesamet. In the UK Nabilone is not licensed for children and young people under 18 years as its efficacy and safety haven’t been established, and it might cause side-effects, such as dizziness, drowsiness, and dry mouth, particularly in children. The use of Nabilone is uncommon in current medical practice, and it is not considered a common treatment for nausea and vomiting caused by chemotherapy. There are no legal requirements regarding Nabilone to be prescribed by a specialist.
Considering that Dravet and Lennox Gastaut syndromes are complicated, difficult kinds of epilepsies with limited effective treatment options, further approval of medical cannabis brought a huge relief. Many parents of children had to pay thousands of pounds per month for medicines with THC and CBD imported from Canada and Europe. These medications resulted in significant reductions in the number and severity of seizures in children.
Even though up to 13% of UK adults suffer from chronic pain, NICE guidelines are not in favour of cannabis-based treatments for pain. The long-term effects of cannabis products or their impact on the developing brain are unknown. It is important to know that cannabis is not a magic bullet, and just like any other anti-seizure medications may not work for some people.
Why is medical cannabis so hard to get?
There are three main hurdles on the way of accessing medical cannabis in the UK:
- There remains a lack of valid clinical data on it’s uses.
- The price of medical cannabis is high due to rather strict and complicated import rules and a lack of supply.
- There’s a widespread lack of training on medical cannabis for doctors in the UK.
Unfortunately, medical cannabis is as expensive as other plant extracts and dried flowers that are imported from countries like Canada and the Netherlands, and due to logistical challenges and o logistical challenges and complicated bureaucratic processes, it’s hard to negotiate lower prices for patients. It’s likely that producing medical cannabis in home soil could help to solve the problem, but currently, this is not a priority for the Home Office.
Due to the limited resources of the NHS, medical guidelines are mostly based on the cost-effectiveness of drugs and treatments rather than their efficacy alone. Following this principle, it’s likely that medical cannabis could be less expensive if the NHS considered it as a treatment for chronic pain. Fortunately, both drugs, Sativex and Epidyolex, were approved partly due to price reduction. But even though guidelines allow them for prescription, local funding bodies may not have enough resources to fund such treatment.
Who is eligible for prescriptions?
Medical cannabis on the NHS is recommended in highly limited circumstances. It is likely to be prescribed for the following groups:

- Children and adults with rare and severe epilepsy.
- Adults with chemotherapy-induced vomiting or nausea.
- People with multiple sclerosis-induced muscle stiffness and spasms.
Medical cannabis is considered by doctors when other treatments are not suitable or helpful. Due to a limited amount of approved medications and strict requirements about who can have access to them, very few people in the UK are likely to get a prescription for medical cannabis. Though it may be frustrating for many people, it is important not to self-medicate with the black market and illegal cannabis. Both THC and CBD can interact with medications, making their effect stronger or weaker, which can worsen the health condition or result in an overdose.
Private doctors can deviate from official guidelines and issue prescriptions in a broader range of conditions. Therefore, more prescriptions for medical cannabis come from independent doctors. Private cannabis prescriptions cost from hundreds to thousands of pounds per month. For that reason, a bit more than a hundred prescriptions are issued per year.
How to access medical cannabis privately
The demand for cannabis-based medicines has never been more evident than after the release of a 2019 YouGov poll, showing that 1.4 million British citizens (2.8% of the adult population) were illegally using ‘street’ cannabis to alleviate chronic health conditions.
Since the legalisation in November 2018, there have been a few prescriptions for medical cannabis, especially with THC content, on the NHS. Access to medical cannabis via the NHS remains difficult and rare in the UK. Therefore, private clinics offer patients a much easier route to access medical cannabis. Moreover, specialists from private clinics may cover a broader range of conditions including cancer, pain, fibromyalgia epilepsy, psychiatric and neurological conditions.
Unfortunately, an easier route is costly and is available to patients who can afford £200-250 for private appointments and between £600-800 for prescriptions per month. As of February 2020, the price for prescriptions could reach up to £3,500 a month.

Private centres
The Medical Cannabis Clinics
Tel: 02039282813
There is a chain of clinics located in London, Birmingham, Manchester, Nottingham, Leeds, Bristol, and Newcastle. The clinic offers the leading cannabis-based therapy and cares for patients with chronic pain, neurological and psychiatric conditions. The team includes multidisciplinary medical cannabis practitioners, experienced and respected cannabinoid experts. Clinics provide cannabis-based therapy for patients suffering from pain, neurological and psychiatric conditions and symptoms, where existing treatments have not proven effective. The Medical Cannabis Clinics were registered with the Care Quality Commission (CQC), the independent regulator of health and social care in England. A referral letter is welcomed, as it allows The Medical Cannabis Clinic specialist to understand more about the health condition, symptoms and treatment history from healthcare professionals involved in patient’s care. If there is no referral letter, a patient will be asked to complete the questionnaire and provide a 10-year medical summary, blood tests results and any letters from specialists overseeing his care. There are also designated discounted appointment slots, and standardised low-cost prescriptions are available. The clinic offers video consultations during the COVID-19 quarantine. Prescriptions take from a few days to up to 28 days.
Sapphire Medical
Tel: 02074594075
Sapphire Medical Clinics aim to provide access to medicinal cannabis for patients who may get clinical benefits via consultation with expert doctors working under the standards of all relevant regulatory authorities. The clinic aims to become a trusted partner of NHS medical professionals and help patients all over the UK in using medicinal cannabis where appropriate. The clinic offers help to patients with cancer-related conditions, gastrointestinal, pain, neurological and psychiatric conditions and in case of palliative care. Sapphire Medical works on a clinician referral program, which means a GP or consultant needs to refer a patient to Sapphire. The clinic unites a multidisciplinary team of clinicians that see patients based on their major condition expertise and speciality. The clinics are registered with the Care Quality Commission (CQC) and offer video consultations.
Cannabis Access Clinics
Tel: 02039980115
Cannabis Access Clinics provides patients in the UK with access to specialist doctors experienced in prescribing cannabis-based products. The clinic’s specialists are GMC registered and only prescribe drugs according to their field of expertise and MHRA guidelines. The patients seen in Cannabis Access Clinics are enrolled in research studies and receive ongoing monitoring of treatment. Along with Applied Cannabis Research, the clinic’s program supports patient safety and aims to improve understanding of the advantages and risks related to medical cannabis use. The clinic welcomes referrals from GP’s and healthcare specialists if their patients may benefit from medical cannabis treatments. The doctors may consult patients through video-based telehealth service.
MyAccess Clinics
Tel: 02039834007
MyAccess Clinics support patients from all over the UK in London and Bristol clinics. Their experts provide independent advice on medical cannabis treatments. The clinics offer affordable and supportive care for patients with debilitating conditions, such as neuropathic and chronic pain, generalised anxiety disorder, sleep disorder, attention deficit hyperactivity disorder (ADHD) and post-traumatic stress disorder (PTSD). There is no need in a referral from a doctor to make an appointment, but a patient needs to be under the care of a doctor. Specialists can provide remote assessments via the phone or by video call. The clinic may arrange in-home assessments via domiciliary care arrangements in special circumstances. MyAccess Clinics work under the guidelines of the MHRA, GMC and NHS England. The healthcare team includes specialist consultants and registered nurses. MyAccess Clinics are registered with the Care Quality Commission (CQC).
Cancard
Carly Barton, the UK’s most known advocate for medicinal cannabis law reform, has recently devised the Cancard campaign. Thanks to this project, a cannabis exemption card will help to protect medicinal cannabis patients from legal prosecution in the UK. Approximately 1 million people in the UK may be eligible for the Cancard if they meet the following criteria:
- Have a diagnosis confirmed by the general practitioner (GP) and prescriptions for private use.
- Have taken two types of prescription drugs or rejected these options due to side effects or potential dependence.
- Are unable to afford the private prescription.
- Are required to have a small amount of cannabis to relieve their condition.
- Are at risk of being criminalised.
Eligible health conditions can be checked on Cancard website. The process of getting Cancard includes the following steps:
Registration
A patient needs to register with Cancard and send the application, which includes a passport-style photo and a contact email of the GP.
Contact the GP
The GP needs to confirm the health condition by signing a form received from Cancard. This form is similar to the one that is requested for private health insurance. The patient needs to permit it over the phone.
Wait until the Cancard is released
Those who possess a Cancard, can identify themselves to police as verified medicinal cannabis patients and can demand open-source legal defence from Cancard if needed.
The organization also plans to work with GPs unwilling to support the initiative. Cancard highlights the importance of the GPs involved as the professional assistance will benefit the application process. The NPCC has stated that they will prevent any relations between the Cancard system and recreational users and dealers. Therefore, the campaign does not allow a person to possess illegal drugs or an excessive amount of cannabis.
To sum up, Cancard is a positive trend, which ensures that patients gain broader access to medical cannabis. Medical cannabis patients mustn’t experience stress due to potential prosecution.
Hope for the future

Looking into the future, the UK’s situation with medical cannabis will hopefully improve over time. Alongside the positive impact of Cancard, distributors have started to secure a broader range of products, EU sources of medical cannabis are expected to come online, and medical cannabis costs are finally beginning to fall. Moreover, the amount of clinical data is set to expand, which will increase the number of conditions medical cannabis is authorised to treat. So far, hope does exist for those who are currently locked out of treatment, including parents of children with epilepsy who are having to pay thousands to obtain imported drugs that contain CBD and THC.
In other recent developments, following concerns about the COVID-19 outbreak, the UK government has claimed that patients holding medical cannabis prescriptions will get their medications faster. Delays will be reduced due to the end of the ban on bulk imports of medical cannabis-based products, and now UK companies will now be able to order and stock more medical cannabis products from abroad. This is set to be a large improvement from the previous system which required orders to be made on a patient-by-patient basis and often resulted in month-long delays.
Finally, another ray of hope that’s likely to improve accessibility to medical cannabis in the UK is Project Twenty21, Europe’s first medical cannabis registry. Project Twenty21 aims to provide sufficient evidence on medical cannabis effectiveness towards treating and controlling specific conditions. The project aims to enrol up to 20,000 patients by the end of 2021, forming the largest body of evidence concerning the effectiveness, tolerability and risk/benefit ratio of medical cannabis.
Its purpose is to show policymakers that medical cannabis should be as widely affordable and available, as other common medicines, and it will also support prescribers across the UK to feel more confident in prescribing medical cannabis to patients. The registry findings are likely to make a convincing case for NHS funding, which may be able to provide a light at the end of the tunnel for patients with multiple sclerosis, post-traumatic stress disorder, anxiety disorder, epilepsy, chronic pain, substance use disorder, and Tourette’s syndrome, who are seeking access to medical cannabis to help treat their condition.
FAQ
Is medical cannabis legal in the UK?
Medical cannabis is legal in the UK. The drug was moved from schedule 1 to schedule 2 in November 2018, which enables patients to use it for medical purposes, as long as it’s prescribed by a registered specialist doctor. However, according to current UK law, the recreational use of cannabis is still prohibited.
Who can prescribe medical cannabis in the UK?
As it currently stands, any doctor on GMC specialist register can prescribe medical cannabis. Doctors on these registers normally include hospital consultants, but some GP’s can also prescribe cannabis-derived medications under shared care arrangements with direction from specialists. Typically, you’re more likely to receive a prescription from a doctor working for a medical cannabis clinic, as these healthcare professionals are likely to be more trained in cannabis medicine.
How do I get a prescription for medical cannabis?
Currently, very few people in the UK are likely to get a prescription for medical cannabis. Prescriptions are only granted for children and adults with rare and severe forms of epilepsy, adults with vomiting or nausea caused by chemotherapy, and people with muscle stiffness and spasms caused by multiple sclerosis (MS). However, NHS specialists are legally permitted to prescribe the medicine, so it’s always worth checking in with them.
Is medical cannabis safe?
To date, there have been no reported overdoses due to the consumption of cannabis. However, after taking medical cannabis, it is possible to develop of following side effects: dizziness, intoxication, hallucinations, feelings of nausea, behavioural or mood changes, and weakness. If you experience any of these side effects from cannabis-based medications, it’s important to report them to your medical team.
How is medical cannabis typically administered?
There’s a variation of ways to take medical cannabis. Cannabis-infused oils can be taken sublingually under the tongue, in the form of topical products, capsules, or dried flowers for vaping. Talking to the doctor is the best way to find out the best way to consume medicinal cannabis for your specific condition. Under current UK law, smoking cannabis is not allowed.
Verified by a Healthcare Professional

Anastasiia Myronenko
Anastasiia Myronenko is a Medical Physicist actively practicing in one of the leading cancer centers in Kyiv, Ukraine. She received her master’s degree in Medical Physics at Karazin Kharkiv National University and completed Biological Physics internship at GSI Helmholtz Centre for Heavy Ion Research, Germany. Anastasiia Myronenko specializes in radiation therapy and is a fellow of Ukrainian Association of Medical Physicists.